Contact Us

Aim of PIG - to support earlier identification of patients nearing the end of their life
The GSF Proactive Identification Guidance, previously known as the Prognostic Indicator Guidance, is a practical guide for clinicians enabling earlier recognition of decline for patients considered to be in their final year/s of life. It is a key tool used within the Gold Standards Framework (GSF) Quality Improvements Training Programmes to support earlier identification of patients, enabling better assessment of their needs and planning care in line with their needs and wishes.
This PIG guidance aims to clarify the triggers that help to identify patients earlier, in order that care can be better planned, more proactive, anticipate patients’ needs and take into account their own wishes following a discussion of their choices and preferences (advance care planning discussion). These patients should be included on a supportive/palliative care register in their GP practice, care home or hospital and in many areas these patients are included on a locality register (digital shared information record) or EpaCCS.
|
Definition of End of Life Care |
|
People are ‘approaching the end of life’ when they are likely to die within the next
|
It is recommended that Advance Care Planning discussions are offered to all as early as possible before further decline, including all suggested here, those in care homes or with Covid. See GSF: https://www.goldstandardsframework.org.uk/advance-care-planning
Once identified and included on the register, such patients may be able to receive additional proactive support, leading to better co-ordinated care reflecting their preferences. This is in line with current thinking on shared decision-making processes and the importance of integrating advance care planning discussions into delivery of care. It is based on consideration of people’s needs rather than exact timescales, acknowledging that people need different things at different times. Earlier recognition of possible illness trajectories means their needs can be better anticipated and addressed.
Predicting needs rather than exact prognostication. This is more about meeting needs than giving defined timescales. The focus is on anticipating patients’ likely needs so that the right care can be provided at the right time. This is related to helping people live well in the time remaining, rather than exact prognostication and leads to better proactive care in alignment with preferences.
Those clinical teams undertaking GSF in their different settings (GP Practices, care homes, hospitals etc) use the GSF PIG firstly to identify patients earlier, then a process of better assessment and planning, which includes use the Needs-based Coding to clarify their different needs with specific actions/ tasks for each stage, to enable better proactive coordinated care.
|
What PIG is |
What PIG is not |
|
|
|
Three triggers that suggest that patients are nearing the end of life, used in GSF
|
|
Benefits to patients and carers of early identification |
Benefits to health and social care teams of early identification |
Potential disadvantages of early identification |
|
|
|
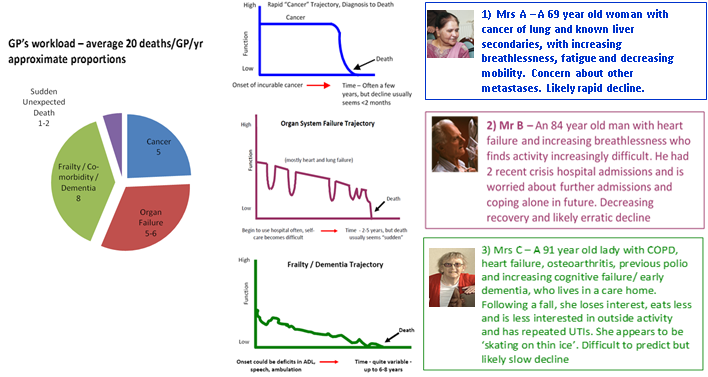
How PIG is used
- In primary care – an estimated 1% of the population dies each year i.e., about 20 patients/GP with an average list size of 2000. This guidance supports early identification by the practice team to consider whether they could be included on the GPs’ Palliative Care/QOF/GSF register and need additional active supportive or palliative care. Once included they are discussed at regular MDT discussions, preferably monthly but at minimum 3 monthly. This is ‘ bronze’ level GSF, mainstreamed to all UK GP practices since 2004. In addition, since 2010, many practices have undertaken the next level GSF Silver or Gold, leading to practice accreditation.
- In hospitals – research would suggest that at any one time 30% of acute hospital inpatients will be in their final year of life (Clarke 2014). However, few hospitals are currently identifying that proportion of patients as being in their final year of life. Hospital teams using GSF however do attain this kind of proportion of early identification of patients, who are then discussed at board rounds/MDT meetings regularly and coded according to needs and phase of illness and an ACP discussion will be initiated.
- In care homes – it is estimated that 80% of nursing care home residents will be in their final year of life. Residents will have their needs assessed and coded on admission and all residents will have had an initial ACP discussion.
- In other settings - PIG is also used in other settings such as hospices, domiciliary care, prisons, etc.
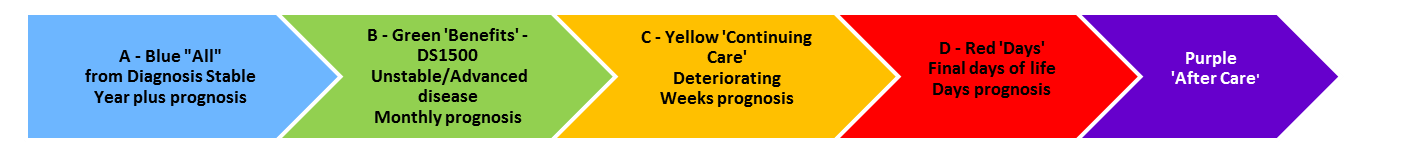
Use of GSF Needs based Coding
Once patients have been identified they have a needs assessment. Needs based coding is used to highlight the level of need by using the red, amber, green (RAG) colour coding system. Red colour coding signifies last days of life, amber – deteriorating, green – decline/ unstable/ advanced disease.
Note - although there is an obvious correlation with timescales and progression of the disease trajectory, this needs-based coding relates to changing needs at different stages to ensure that the patients’ needs are anticipated and met - as in the GSF Programmes, the right person receives the right care at the right time in the right place - every time.
Examples of good practice include
Primary care
- GSF accredited practices identifying 50-90 % of their practice patients who die
- Significant increases in GP practices identifying their patients, from an average of 25% to above 50%
- Initiating Advance Care Planning discussions (ACP) on average 68% the range across the 17 practices (37% - 100%)
Hospitals
- Acute Hospitals on average identifying 34% patients on their wards
- Community hospitals increasing identification rates from 34% to over 60% in some cases
Care Homes
- Identifying and needs-based coding all residents in GSF accredited care homes
For more details of use of GSF PIG in the GSF programmes contact us for more details
info@gsfcentre.co.uk or info@gsfinternational.org.uk


